- Posted On: January 9, 2020
- By: admin
- Share:
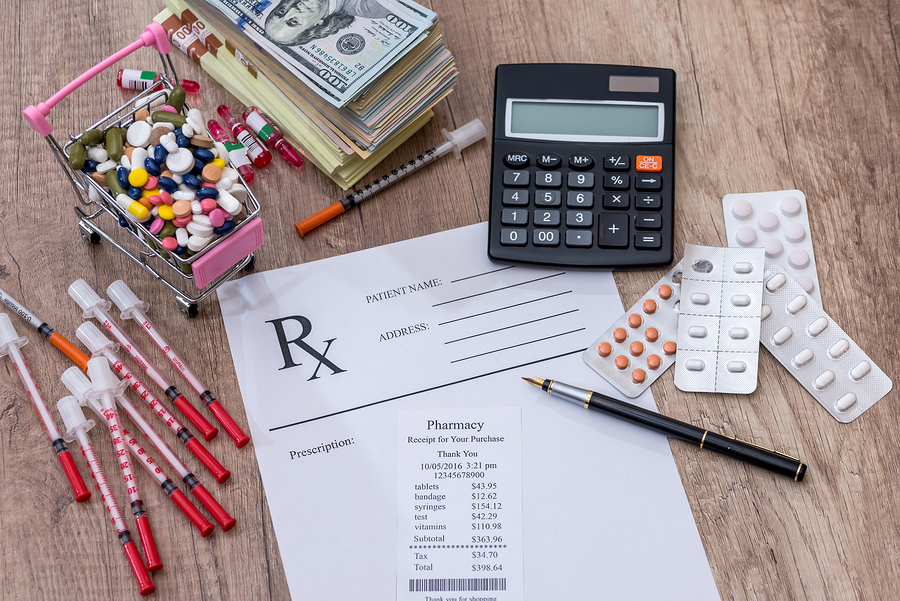
Medications Not Covered – What To Do Now?
Drugs are often dropped from insurance coverage if they are seldom used or if there is a generic or more affordable option available on the market. Medications such as Cambia, Saizen, Uroxatral, Plavix, Mavyret, Tramadol, Viagra, Alocril and many more are currently dropped off from the formulary (drug list) coverage by either or both of the two leading pharmacy benefits managers (PBMs) – Caremark and Express Scripts. Some more medications that you might be taking for years may be dropped in 2020 from your insurance coverage by your plan. Usually, medications for weight loss such as Adipex (Phentermine), cosmetic purposes (such as Renova), fertility (such as Clomid), prescription vitamins and minerals products, devices, medical supplies and bulk chemicals are not covered by the health insurance plans.
If the medication you are taking is dropped from coverage ask your doctor to prescribe a generic or less expensive version of a branded medication. If the medication you need is in your plan’s formulary but it’s on higher-tier or is non-preferred, you can ask your insurer for a tier-exception to help lower your expenses. Tier-1 usually has the medications with the lowest copays, which are mostly generics while Tier-6 or the highest tier of your plan contains medications have the highest copays. You need to be on guard because your medication may be dropped from the formulary or moved to a higher tier in 2020, which will make a big difference to your share of the costs.
You can also apply for patient assistance program if you have no health insurance or a manufacturer co-pay program if you have health insurance. And if you have enrolled for Medicare, use the Plan Finder to find the best plan that suits your needs. You can also consider revaluating your plan during the Enrollment Period to switch to a plan that can cover the medications that you or your family may need often.
You may also file for an exception with your insurer for your uncovered drug, provided your doctor confirms that the particular medication is needed for your specific health condition as other covered drugs or alternatives may not be as effective. If your exception request is accepted, your medication will be treated as covered by your plan, and you will only be charged the copay for the most expensive medication already covered by your plan. In case your exception request is denied, you can still have the decision reviewed by a third party. Your insurer is obliged to inform you about the reasons for the denial. The review decision may take up to 60 days, and you may have to pay $25 if it is handled by your state or an independent review organization. The review is free if handled by the US Department of Health and Human Services (HHS).
If your medication is no longer covered, it’s not the time for open enrollment, your exception appeal is denied and you need a specific medication for yourself or someone else in your family, be prepared to pay out-of-pocket for it, which is usually much higher than your insurance copay.
To help you with these costs, SaveonMeds drug card offers you unmatched benefits for savings on drugs. It is available for free, and accepted at over 65,000 network pharmacies all over the USA to let you make savings on prescriptions of up to 85% on various branded and generic medications.
At savingsonmeds.com, you can also check drug prices at the pharmacies near you. It will show you the lowest price of the medication, which in some cases may be much lower then you’re insurance copay. You will be surprised to know that prescription medication prices vary widely from one pharmacy to the next, even in the same zip code, and you can always look for the lowest price for maximized savings on prescription medicines.
You can save more on prescription costs with SaveonMeds drug discount card as many big pharmacy chains such as Publix, CVS, Target, Walgreens offer hundreds of generics for as low as $4 for a 30-day supply, and $10 for a 90-day supply. Ask for a 90-day supply to see if the copays are lower.
To get your digital drug savings card, text the keyword “SAVEONMEDS” to 21000 from your mobile or simply download your activated prescription card from www.savingsonmeds.com for FREE. You can use it as a flu vaccine discount card, Albuterol discount card, and Adipex savings card, and to help every member of your family and friends to save on prescription medications.
Disclaimer: The information and content posted on this website is intended for informational purposes only and is not intended to be used as a replacement for medical advice. Always seek medical advice from a medical professional for diagnosis or treatment, including before embarking on and/or changing any prescription medication or for specific medical advice related to your medical history.
Click here to download your card